Antonio Inserria
Ayahuasca ingestion modulates brain activity, neurotransmission, gene expression and epigenetic regulation. N,N-Dimethyltryptamine (DMT, one of the alkaloids in Ayahuasca) activates sigma 1 receptor (SIGMAR1) and others. SIGMAR1 is a multi-faceted stress-responsive receptor which promotes cell survival, neuroprotection, neuroplasticity, and neuroimmunomodulation. Simultaneously, monoamine oxidase inhibitors (MAOIs) also present in Ayahuasca prevent the degradation of DMT. One peculiarity of SIGMAR1 activation and MAOI activity is the reversal of mnemonic deficits in pre-clinical models. Since traumatic memories in post-traumatic stress disorder (PTSD) are often characterised by “repression” and PTSD patients ingesting Ayahuasca report the retrieval of such memories, it cannot be excluded that DMT-mediated SIGMAR1 activation and the concomitant MAOIs effects during Ayahuasca ingestion might mediate such “anti-amnesic” process. Here I hypothesise that Ayahuasca, via hyperactivation of trauma and emotional memory-related centres, and via its concomitant SIGMAR1- and MAOIs- induced anti-amnesic effects, facilitates the retrieval of traumatic memories, in turn making them labile (destabilised). As Ayahuasca alkaloids enhance synaptic plasticity, increase neurogenesis and boost dopaminergic neurotransmission, and those processes are involved in memory reconsolidation and fear extinction, the fear response triggered by the memory can be reprogramed and/or extinguished. Subsequently, the memory is stored with this updated significance. To date, it is unclear if new memories replace, co-exist with or bypass old ones. Although the mechanisms involved in memory are still debated, they seem to require the involvement of cellular and molecular events, such as reorganisation of homo and heteroreceptor complexes at the synapse, synaptic plasticity, and epigenetic re-modulation of gene expression. Since SIGMAR1 mobilises synaptic receptor, boosts synaptic plasticity and modulates epigenetic processes, such effects might be involved in the reported healing of traumatic memories in PTSD patients. If this theory proves to be true, Ayahuasca could come to represent the only standing pharmacological treatment which targets traumatic memories in PTSD. Lastly, since SIGMAR1 activation triggers both epigenetic and immunomodulatory programmes, the mechanism here presented could help understanding and treating other conditions in which the cellular memory is dysregulated, such as cancer, diabetes, autoimmune and neurodegenerative pathologies and substance addiction.
Introduction
Ayahuasca is a psychoactive plant brew containing N,N-dimethyltryptamine (DMT) and β-carboline alkaloids (harmine, harmaline, and tetrahydroharmine) traditionally used in the Amazon basin for therapeutic and spiritual purposes (Schultes et al., 1979; Frecska et al., 2016). The hallucinogenic tryptamine DMT is obtained from Psychotria viridis and it binds to SIGMAR1, the serotonin receptors (5HTR) 1A/1D/1E/2A/2B/2C/5A/6/7, the serotonin transporter, the dopamine receptor D1 (D1R), the adrenergic receptors alpha 1A/1B/2A/2B/2C, the imidazoline 1 receptor and the trace amine associated receptor (Deliganis et al., 1991; Smith et al., 1998; Bunzow et al., 2001; Fontanilla et al., 2009; Ray, 2010). β-carbolines are obtained from Banisteriopsis caapi and function as monoamine oxidase inhibitors (MAOIs) to render DMT orally active (Riba et al., 2003).
Ayahuasca seems to hold therapeutic potential in psychiatry. Recently, fast onset antidepressant effects were reported following administration of a single dose of Ayahuasca in patients diagnosed with recurrent depression (Sanches et al., 2016). Similarly, anecdotal evidence suggests that Ayahuasca might be beneficial in the treatment of post-traumatic stress disorder (PTSD) (Nielson and Megler, 2014). However, no pre-clinical or clinical studies to date have investigated this possibility.
In this work, based on converging layers of evidence from in-vitro, pre-clinical and clinical studies, I postulate a mechanism involving the activation of discrete brain areas and receptor systems which triggers the recall of traumatic memories and their reconsolidation (and potentially fear extinction learning) hypothetically via modifying the epigenetic signatures of the memory.
Go to:
Ayahuasca Ingestion Modulates Brain Activity
The deep changes in perception and cognition elicited by Ayahuasca ingestion are underlined by a profound activation of limbic, paralimbic and neocortical brain areas, which are involved in trauma, memory formation, memory retrieval and emotional regulation, as well as a region-specific shift of electrical activity. These changes lead to an altered state of awareness underlined by introspection, retrieval of traumatic memories, and visions. Imaging studies have shown that Ayahuasca hyperactivates the inferior frontal gyrus (IFG) and the anterior insula, the right anterior cingulate/subcallosal gyrus and the left amygdala/parahippocampal gyrus, while decreasing activity within relevant hubs of the default mode network (DMN), such as the precuneus/posterior cingulate cortex and the medial prefrontal cortex (Riba et al., 2006; Palhano-Fontes et al., 2015).
The inferior frontal gyrus (IFG) is a brain area involved in semantic unification, emotion perception and regulation and processing of negative emotional stimuli (Etkin et al., 2011; Zhu et al., 2012; Tabei, 2015; Urgesi et al., 2016). This suggests that activation of this brain area during Ayahuasca ingestion could be involved in the processing of trauma. Significantly, veterans diagnosed with PTSD display decreased IFG activation in response to contextual cues, suggesting that modulation of this brain area might be beneficial in PTSD treatment (van Rooij et al., 2014). Similarly, the anterior insula is hyperactivated following Ayahuasca ingestion, and this region is involved in emotional processing and in the conscious perception of errors (Phillips et al., 1998; Ullsperger et al., 2010). The amygdala is involved in fear response, emotional arousal processes, reconsolidation of fear memories and fear memory extinction, and this brain region has been shown to be hyper-responsive in PTSD (Riba et al., 2006; Shin et al., 2006; Myers and Davis, 2007; Palhano-Fontes et al., 2015). Ayahuasca-induced hyperactivity of this brain area therefore supports the processing and reconsolidation of traumatic memories and the extinction of the fear memory associated with recall of the traumatic memory (Riba et al., 2006; Shin et al., 2006; Myers and Davis, 2007; Palhano-Fontes et al., 2015).
The subcallosal gyrus is involved in the processing of sadness and sad memories (Mayberg et al., 1999). Increased activity of this brain region is observed when patients are asked to rehearse sad autobiographic scripts, in line with the hypothesis presented here. Significantly, co-activation of the IFG, amygdala and hippocampus is a prerequisite for autobiographical memory retrieval, and specific sub-regions of these brain areas are activated following Ayahuasca ingestion (Greenberg et al., 2005; Riba et al., 2006). Moreover, parahippocampal gyrus activity is increased during memory retrieval tasks, and Ayahuasca hyperactivates this brain area (Maguire and Mummery, 1999).
Much like other psychedelic compounds such as psilocybin and lysergic acid diethylamide (LSD), Ayahuasca ingestion dampens activity and connectivity of crucial hubs within the DMN, such as the precuneus/posterior cingulate cortex and the medial prefrontal cortex (Carhart-Harris et al., 2012; Palhano-Fontes et al., 2015; Speth et al., 2016). Of relevance, the medial prefrontal cortex is involved in the process of fear extinction, and its activity is modulated by Ayahuasca (Myers and Davis, 2007; Palhano-Fontes et al., 2015).
Go to:
Ayahuasca Ingestion Modulates Neurotransmission
To date, only one study has investigated the effects of Ayahuasca administration on neurotransmission (de Castro-Neto et al., 2013). In this study, the authors orally administered rats three Ayahuasca doses and studied post-mortem amino acid and monoamines levels in the hippocampus and amygdala. Gamma-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the human brain, was dose-independently increased in the hippocampus while it was increased in the amygdala at the lowest dose and decreased at the highest concentrations. Moreover, in the amygdala, noradrenaline, serotonin and dopamine levels were increased at all doses studied, while in the hippocampus only serotonin was increased in rats receiving the two highest doses. Furthermore, the turnover of serotonin, noradrenaline and dopamine was drastically reduced in the amygdala but not in the hippocampus of Ayahuasca-treated rats (de Castro-Neto et al., 2013).
These findings suggest that Ayahuasca ingestion exerts profound monoaminergic effects in the amygdala, increasing the levels of excitatory and decreasing those of inhibitory neurotransmitters, while decreasing monoamine utilisation. The findings that GABA is decreased and dopamine is increased in the amygdala following Ayahuasca administration is relevant for the hypothesis here presented, since the GABAergic system mediates the amnesic effects of chemical compounds, and negative modulation of the GABAergic system has anti-amnesic effects, while amygdalar dopamine is involved in the extinction of conditioned fear (Rau et al., 2009; Abraham et al., 2014). Thus, the decreased levels of amygdalar GABA might be at least partially responsible for the anti-amnesic-like effects of Ayahuasca on the retrieval of repressed memories in PTSD patients, while the increased levels of amygdalar dopamine might play an important role in the process of fear extinction (discussed below).
Further studies should investigate if similar changes in neurotransmission are replicable in humans. This could be possible via in vivo approaches, by using neuroimaging techniques to a) directly measure the levels of neurotransmitter release following Ayahuasca ingestion or b) indirectly, by measuring the relative drug occupancy at receptors for each of the neurotransmitter of interest (Badgaiyan, 2014; Kumar and Mann, 2014). However, until otherwise proven, it seems likely that Ayahuasca ingestion might trigger similar neurotransmission patterns in humans. These changes could be involved in the reported antidepressant effects of Ayahuasca and in the anecdotal reports of Ayahuasca consumption in the healing of trauma (Dominguez-Clave et al., 2016; Sanches et al., 2016).
Go to:
Ayahuasca Ingestion Modulates Neurogenesis
Aside from their monoaminergic effects, the alkaloids present in Ayahuasca have been shown to increase neurogenesis in vitro and in vivo at least partially via SIGMAR1-mediated upregulation of brain-derived neurotrophic factor (BDNF) (Fortunato et al., 2009; Fujimoto et al., 2012; Lenart et al., 2016; Morales-Garcia et al., 2017). The processes of memory reconsolidation and fear extinction (discussed below) both require synaptic plasticity enhancement and hippocampal neurogenesis, which are modulated by BDNF (Radiske et al., 2015; Suarez-Pereira and Carrion, 2015). Therefore, it seems likely that the Ayahuasca-induced synaptic plasticity and neurogenesis, which are required for mnemonic processes and fear extinction, might be involved in the healing of traumatic memories experienced by Ayahuasca users.
Go to:
Sigma-1 Receptor
SIGMAR1 is a transmembrane protein with neuroprotective, neurotrophic, and immunomodulatory properties found in high concentrations in limbic areas of the human brain and in immune cells (Ishikawa et al., 2007; Fujimoto et al., 2012; Frecska et al., 2013; Szabo et al., 2014). SIGMAR1 can be membrane-bound at the mitochondria-associated endoplasmic reticulum (ER) membrane, where it acts as a molecular chaperone, or translocate to the nuclear envelope, the cytosol and the plasma membrane. (Hayashi and Su, 2007; Tsai et al., 2015). At the nuclear envelope, SIGMAR1 recruits chromatin-remodelling molecules to control gene expression (Tsai et al., 2015). Aside from its effects at the ER and nuclear level, SIGMAR1 also plays an important role at the synaptic level both via forming heteroreceptor complexes with G-protein coupled receptors (GPCRs) and via directly interacting with voltage-gated ion channels, therefore controlling the reorganisation of several homo and heteroreceptor complexes and modulating neurotransmission. (Kourrich et al., 2013; Balasuriya et al., 2014; Beggiato et al., 2017; Feltmann et al., 2018; Ortiz-Renteria et al., 2018) Dysregulation of SIGMAR1 function is implicated in neuropsychiatric and neurodegenerative disorders, drug addiction, cancer, cardiovascular diseases, immune-related pathologies, stroke and neuropathic pain [Reviewed in (Tsai et al., 2009; Frecska et al., 2016)].
One peculiarity of the human SIGMAR1 gene is that, unlike any other, it only shares 30.3% homology with any other mammalian protein, while sharing 66.7% identity with the enzyme sterol isomerase found in fungi, which is involved in the biosynthesis of ergosterol (Hanner et al., 1996; Weete et al., 2010). Ergosterol is a compound found in the cell membrane of fungi and protozoa first identified in the fungus Claviceps Purpurea (Weete et al., 2010). Interestingly, this fungus produces ergot alkaloids amongst which lysergic acid, a precursor of the synthetic LSD (Miedaner and Geiger, 2015). Some authors have suggested that, unlike the traditional view that 5HT receptors mediate the psychedelic effects of tryptamines, SIGMAR1 might also be involved in those effects (Fontanilla et al., 2009). Although such discussion is beyond the scope of this work and shall be argued elsewhere, the author believes that SIGMAR1 might represent the real gateway to psychedelic states. Further studies should investigate this possibility.
Sigma 1 Receptor Activation Is Anti-amnesic
Aside from its neuroprotective and immunomodulatory properties, SIGMAR1 activation has been shown to reverse experimental-induced amnesia in rodents, possibly via enhancement of the cholinergic and N-methyl-d-aspartate- (NMDA) glutamatergic neurotransmitter systems (Earley et al., 1991; Maurice et al., 1998; Antonini et al., 2009). Interestingly, peak densities of SIGMAR1 are found in brain areas relevant to traumatic memory formation, retrieval and updating, such as the amygdala and the hippocampal formation, suggesting that Ayahuasca-induced SIGMAR1 activation in such brain areas could be involved in the reported retrieval and updating of traumatic memories (Mash and Zabetian, 1992). Supporting this notion, the parahippocampal gyrus, one of the brain areas hyperactivated by Ayahuasca ingestion, is involved in the modulation of memory retrieval (Woodcock et al., 2015).
Accordingly, SIGMAR1, D2R and 5HT2AR are enriched in the amygdala, while SIGMAR1-D2R and D2R-5HT2AR have been shown to interact to form heteroreceptor complexes at the post-junctional membrane of synapses. (Beggiato et al., 2017; Feltmann et al., 2018) The term “junctional neurotransmission” identifies a type of neurotransmission which is “non-synaptic” and refers to the neurotransmission at neuro-non-neural effectors, that is the connexion between neuronal and non-neuronal cells (such as smooth muscle cells). Such non-synaptic neurotransmission is achieved by means of GPCRs metabotropic receptors signalling, and produces a slower (second to minutes) response compared to synaptic neurotransmission. (Goyal and Chaudhury, 2013) Given that (a) SIGMAR1 plays an important role in junctional neurotransmission via forming heteroreceptor complexes with other metabotropic receptors such as 5HT2AR and D2R and that (b) DMT has high affinity for SIGMAR1 and 5HT2AR, and the latter forms heteroreceptor complexes with both SIGMAR1 and D2R, and that (c) D2R-5HT2AR oligomerization enhances D2R promoter recognition and signalling, it could be plausible that this mechanisms at the post-junctional synapse might enhance the effects of DMT on dopaminergic neurotransmission in the amygdala, a crucial event in memory retrieval and reconsolidation. (Borroto-Escuela et al., 2010, 2014, 2017; Lukasiewicz et al., 2010; Albizu et al., 2011)
Therefore, it seems possible that the elicited patterns of brain activation arising from Ayahuasca ingestion, accompanied by the DMT-induced SIGMAR1 activation leading to gene expression regulation, and by the formation of heteroreceptor complexes to boost dopaminergic neurotransmission, might mediate the retrieval of repressed traumatic memories. This kind of retrieval process forms an essential step in the re-elaboration and re-contextualization of such memories. Interestingly, MAOI activity has also been shown to be beneficial in pre-clinical models of amnesia, and Ayahuasca contains MAOIs (Botwinick and Quartermain, 1974).
Sigma 1 Receptor Activation Modulates Epigenetic Processes
Recently, SIGMAR1 has been shown to modulate epigenetic processes. In fact, cocaine-induced SIGMAR1 activation triggers SIGMAR1 translocation to the nuclear envelope, where it interacts with proteins which regulate gene expression by affecting chromatin compaction (Tsai et al., 2015). Specifically, SIGMAR1 was shown to create a dose-dependent interaction between emerin and histone deacetylase (HDAC) 1, HDAC2 and HDAC3 and to therefore affect chromatin compaction and gene expression (Demmerle et al., 2012; Tsai et al., 2015). Therefore, for the first time, a study has described an involvement of SIGMAR1 on the epigenetic regulation of gene expression. This is in line with the hypothesis here presented, since reconsolidation and fear extinction of traumatic memories both seem to require the involvement of epigenetic mechanisms (Graff et al., 2014; Kwapis and Wood, 2014).
Sigma 1 Receptor Activation Disrupts the Reconsolidation of Fear Memories
Aside from promoting anti-amnesic and regulating epigenetic intracellular pathways, activated SIGMAR1 modulates the cannabinoid receptor 1 (CB1)/NMDA receptor interaction to prevent NMDA receptor dysfunction (Sanchez-Blazquez et al., 2014). In support of the hypothesis here presented, CB1 receptors are enriched in the basolateral amygdala (a region involved in conditioned fear), and pharmacological agonists that activate CB1 or NMDA receptors during traumatic memory retrieval disrupt the reconsolidation of fear memories, preventing subsequent fear expression (McDonald and Mascagni, 2001; Lee et al., 2017). This mechanism could be involved in the extinction of fear memory and healing of traumatic memories reported by Ayahuasca users (Nielson and Megler, 2014).
Go to:
Memory, Ptsd and Traumatic Memories
Memory formation is the ensemble of highly dynamic processes that permit specific aspects of an event to be stored in the brain (Nadel et al., 2012). The mechanisms involved in memory formation, retrieval and reconsolidation have long been investigated. However, because of the highly complex nature of such processes, and because of the difficulties in studying them, the exact nature of these mechanisms are still debated. It is, however, accepted that mnemonic processes (i.e., memory consolidation, retrieval and reconsolidation) require the involvement of cellular and molecular mechanisms, such as synaptic plasticity and the transcriptional modulation of specific sets of genes in relevant neuronal subpopulations, which are likely to be mediated by epigenetic modifications (Jarome and Lubin, 2014).
Several hypotheses have been formulated trying to describe the elusive mechanisms of memory formation, retrieval and reconsolidation. Although diverging in some aspects, these hypotheses are not necessarily mutually exclusive, and they could hold the key to explain slightly different mechanisms of the same paradigm. The “synaptic plasticity” hypothesis suggests that activity-dependent plasticity is achieved at appropriate synapses and is necessary and sufficient for storage, retrieval and reconsolidation of the memory engram. (Martin et al., 2000; Takeuchi et al., 2014) The “memory indexing theory” or “hippocampal hypothesis of memory,” suggests that the pattern of neocortical and other brain areas activated by an event are initially indexed (i.e., “photographed”) in the hippocampus only to be subsequently stored in other brain regions, such as the neocortex. (Teyler and DiScenna, 1985) The “consolidation hypothesis” disputes that new memories consolidate slowly over time unless new information is learnt shortly after the initial learning. (McGaugh, 2000) The “cholinergic hypothesis” proposes that cholinergic neurons are central player in the formation and storage of memory, and that cholinergic dysfunction is involved in memory and cognitive deficits. (Bartus et al., 1982; Contestabile, 2011) The “vasopressin hypothesis” argues that vasopressin is the fundamental peptide that enhances memory given that vasopressin delayed memory extinction. (Strupp and Levitsky, 1985) The “fragmentation hypothesis” holds that a specific memory is stored as fragments of the specific perceived situation. It has been suggested that this mechanisms might be relevant to PTSD via the phenomenon of “dissociative encoding”, the insufficient encoding of the trauma memory following peritraumatic dissociation which prevents future re-elaboration of the traumatic memory (Bedard-Gilligan and Zoellner, 2012).
Nonetheless, some authors have suggested that long-term memory might be mediated by the allosteric reorganisation of populations of homo- and heteroreceptor complexes in the post-junctional membranes, which in turn affect the pre-junctional receptor complexes to facilitate the new pattern of transmitter release to be learned. (Borroto-Escuela et al., 2015, 2017; Fuxe and Borroto-Escuela, 2016b) Specifically, the transformation of sub-regions of heteroreceptor complexes into transcription factors, upon formation of specific adapter proteins, can consolidate the heteroreceptor complexes into long-term units. Those influence gene expression via altered promoter recognition, signalling and trafficking as well as via the formation of novel allosteric sites, which can lead to changes in promoter function and pharmacology. (Fuxe and Borroto-Escuela, 2016a; Borroto-Escuela et al., 2017) Hence, given that SIGMAR1 controls the reorganisational pattern of several homo- and heteroreceptor complexes at the synapses, it cannot be excluded that these mechanisms might be involved in the reported retrieval and healing of traumatic memories following DMT-mediated SIGMAR1 activation. This might result in a “new post-junctional transmission learning” mediated by a long term modulation of the neuronal networks in which the memory is encoded. Further studies are warranted to explore this possibility.
Traumatic Memories and Brain Activity in PTSD
When a traumatic event is experienced, the extent of circulating glucocorticoids and adrenalin seem to determine the formation fate of a memory of the event. For example, when the stressor is particularly intense and the levels of stress hormones (such as glucocorticoids) become particularly elevated, formation of the memory can be impaired [Reviewed by (Schwabe et al., 2010)]. Following such events, deficits in declarative memory (the difficulty of recalling the traumatic event) can be experienced (Samuelson, 2011). Exposure to highly traumatic situations can lead to the development of PTSD, a disorder characterised by intrusive thoughts, repression of trauma memory, flashbacks, nightmares, hyperarousal, startle response, and changes in memory and concentration (Bremner, 2006).
Individuals diagnosed with PTSD display changes in brain function and structure, such as alterations of the hippocampus, amygdala and medial prefrontal cortex (including anterior cingulate cortex). Crucially, Ayahuasca ingestion modulates activity of these brain areas (Bremner et al., 1997; Lanius et al., 2001; Bremner, 2006; Riba et al., 2006; Palhano-Fontes et al., 2015). Human studies suggest that PTSD patients present disorder-specific epigenetic regulation of genes involved in pathways relevant to this disorder (Zannas et al., 2015). Given that SIGMAR1 activation is involved in chromatin remodelling and epigenetics regulation of gene expression, it cannot be excluded that DMT-mediated SIGMAR1 activation might affect aberrant gene expression and/or epigenetic signatures in PTSD.
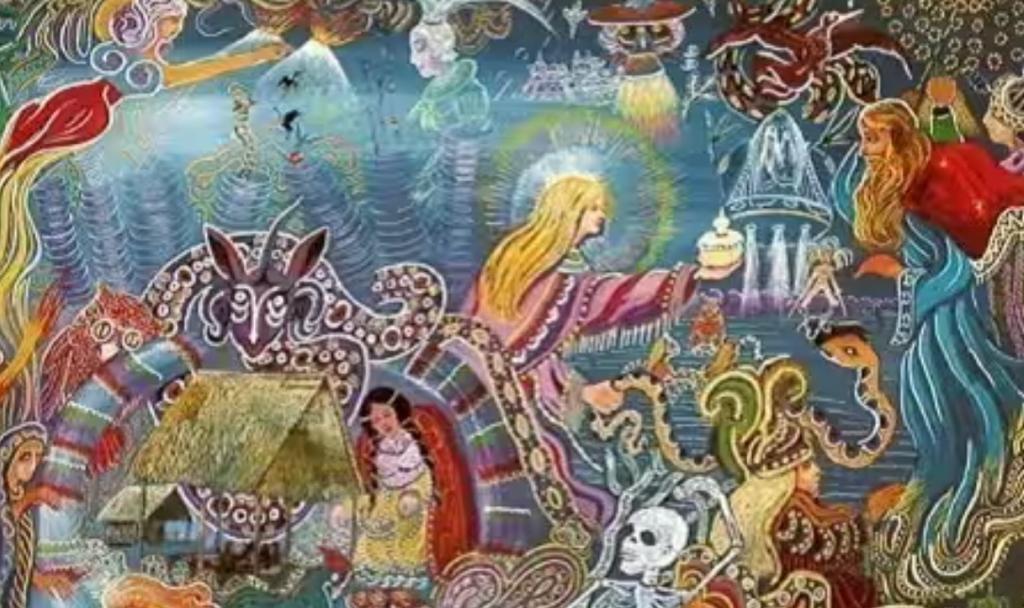
Ayahuasca Retreat Iquitos
Ayahuasca Peru
Best Ayahuasca Retreat
Flower of life Ayahuasca Healing Center
Shamanic course Peru
If you feel called, join us for a transformational Medicinal Plants Retreat Program at Flower of Life Ayahuasca Healing Center in Peru.
We will be delighted to have you in a safe and nurturing environment in the Amazonian Rainforest in Peru.
WhatsApp + 1 786 393 0799
www.floweroflifeperu.com